Peroral Endoscopic Myotomy for End-Stage Achalasia: challenge accepted!
Luís Santos1, Carlos Borges Chaves1, Marta Gravito-Soares1,2, Elisa Gravito-Soares1,2, Paulo Souto1, Pedro Amaro1, Pedro Figueiredo1,2
1 Gastroenterology Department, Centro Hospitalar e Universitário de Coimbra, Unidade Local de Saúde de Coimbra, Coimbra, Portugal
2 Faculty of Medicine, University of Coimbra, Coimbra, Portugal
DESCRIPTION
A 47-year-old man with end-stage achalasia presented with progressive dysphagia, retrosternal chest pain, and weight loss (Eckardt score 5). Previous treatments were unsuccessful, including multiple endoscopic pneumatic dilations (PD). A re-evaluation barium esophagogram showed the typical bird’s beak appearance and a dilated, tortuous, sigmoid-type esophagus with a maximum diameter of 8 cm (Figure 1).
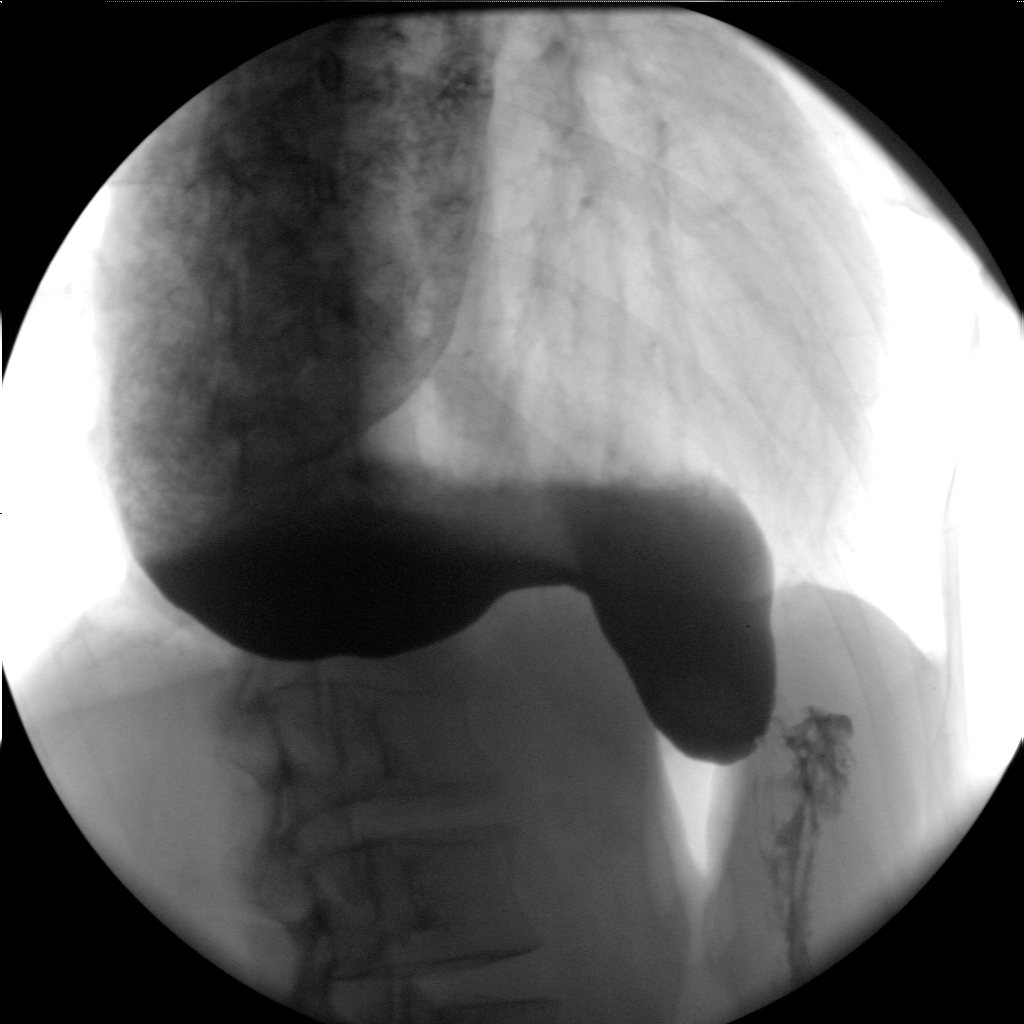
Figure.1 Barium swallow shows a sigmoid-shaped esophagus with a maximum diameter of 8 cm (stage 4).
After multidisciplinary discussion, the patient was proposed for peroral endoscopic myotomy (POEM). The endoscopic appearance revealed a widened esophagus with a pansigmoid conformation (Figure 2-A). A first attempt through a posterior mucosoctomy (5 o’clock position; Figure 2-B) was not possible due to intense fibrosis replacing the entire submucosa, precluding submucosal tunneling. Therefore, a second mucosoctomy was performed using an anterior approach (2 o’clock position; Figure 2-C), enabling adequate submucosal tunneling (Figure 2-D). The maintenance of the appropriate tunneling axis was ensured by repeatedly identifying the luminal direction of bluish elevation towards the lower esophageal sphincter (LES). Following, the myotomy was performed (Figure 2-E) and the mucosoctomy sites were closed (Figure 2-F), without intercurrences. Patient was discharged after 72 hours and had an uneventful recovery. At 6 months of follow-up, he remained asymptomatic (Eckardt score 0).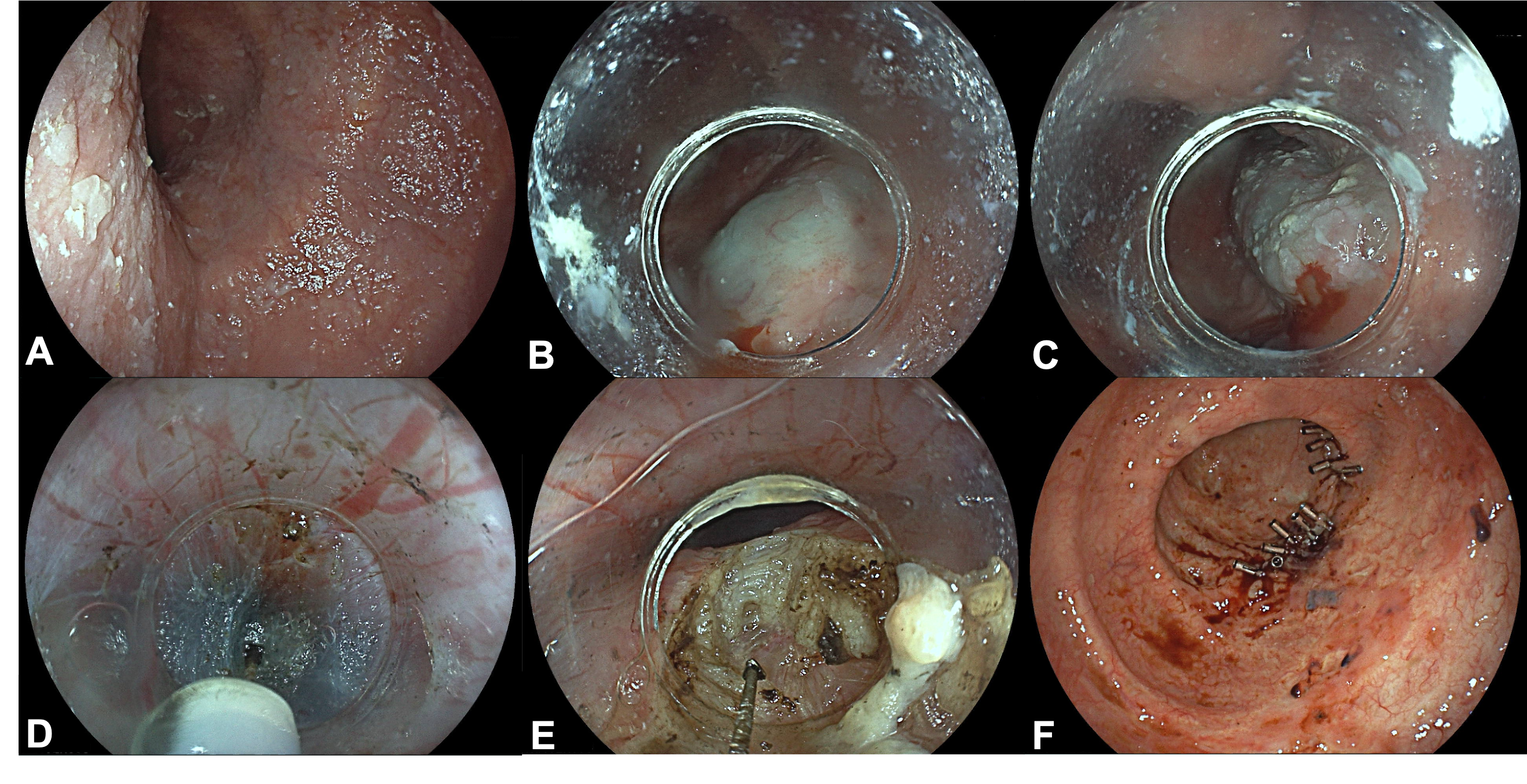 Figure. 2 (A) Gastroscopy revealing a severe dilated and tortuous esophageal lumen; (B) Posterior mucosoctomy site (5 o’clock position); (C) Anterior mucosoctomy site (2 o’clock position); (D) Submucosal tunnelling using the Triangle Tip Knife J (Olympus, Tokyo, Japan); (E) Lower esophageal sphincter myotomy using the Triangle Tip Knife J (Olympus, Tokyo, Japan); (F) Closure of both mucosal entry incisions with through-the-scope clips.
Figure. 2 (A) Gastroscopy revealing a severe dilated and tortuous esophageal lumen; (B) Posterior mucosoctomy site (5 o’clock position); (C) Anterior mucosoctomy site (2 o’clock position); (D) Submucosal tunnelling using the Triangle Tip Knife J (Olympus, Tokyo, Japan); (E) Lower esophageal sphincter myotomy using the Triangle Tip Knife J (Olympus, Tokyo, Japan); (F) Closure of both mucosal entry incisions with through-the-scope clips.
DISCUSSION
Achalasia, the most frequent and best-studied primary motor disorder of the esophagus, is clinically characterized by cardinal symptoms such as dysphagia, regurgitation, and weight loss. Chest pain can also be present. These symptoms are primarily due to aperistalsis of the esophageal body and impaired relaxation of the LES1,2. The goal of managing achalasia is to improve symptoms by decreasing the pressure gradient of the LES to enhance the esophageal emptying. Over the past two decades, the treatment landscape has undergone significant advances. Current therapeutic strategies include endoscopic botulinum toxin injection (BTI), PD, laparoscopic Heller myotomy (LHM), and POEM3. Nevertheless, there is still no cure, and around 10-15% of patients will eventually advance to end-stage achalasia. This stage is typified by severe dysphagia and weight loss, accompanied by significant esophageal dilation and tortuosity, leading to a loss of its normal shape and the development of a sigmoid-like esophagus or megaesophagus1. Traditionally, LHM or esophagectomy were considered the mainstay of advanced achalasia treatment. In the last years, POEM has emerged as a minimally-invasive alternative in such cases, offering excellent outcomes along with favorable safety and efficacy4,5. Despite that, in cases of end-stage achalasia, performing POEM may pose technical difficulties due to morphological alterations in the esophagus. These changes can make this technique more challenging and time-consuming, raising the risk of complications. In this setting, a wider tunnel to pass through the twists, a shorter tunnel with myotomy close to the mucosoctomy, repeated luminal visualization of the correct tunnel direction towards the LES, tunneling under fluoroscopy, and in cases of intense fibrosis, changing the approach position with less fibrosis and possible dissection of the submucosa/muscle during tunneling can be tips and tricks to overcome these endoscopic challenges6. Our report highlights the efficacy and safety of POEM in treating achalasia, even in the end-stage disease with the presence of significant submucosal fibrosis.
REFERENCES
1. Duranceau A, Liberman M, Martin J, Ferraro P. End-stage achalasia. Dis Esophagus 2012;25(4):319-330.
2. Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol 2020;115(9):1393-1411
3. Mundre P, Black CJ, Mohammed N, Ford AC. Efficacy of surgical or endoscopic treatment of idiopathic achalasia: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol 2021;6(1):30-38.
4. Nabi Z, Ramchandani M, Basha J, Goud R, Darisetty S, Reddy DN. Outcomes of Per-oral Endoscopic Myotomy in Sigmoid and Advanced Sigmoid Achalasia. J Gastrointest Surg 2021;25(2):530-532.
5. Qiu S, Chai N, Zhai Y, Wang X, Wang Y, Linghu E. Advanced achalasia: good candidate for peroral endoscopic myotomy. Dis Esophagus 2021;34(3):doaa097.
6. Mandavdhare HS, Samanta J, Jafra A, Singh H, Gupta P, Dutta U. Outcome of per oral endoscopic myotomy (POEM) in sigmoid achalasia at a median follow up of 17 months. Arq Gastroenterol 2022;59(4):478-482.


